How to Choose the Right Medical Billing Company
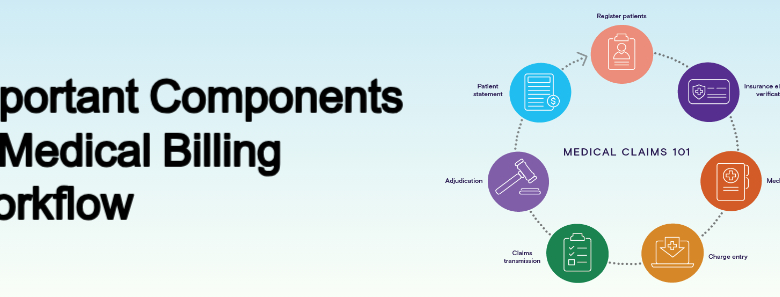
Introduction Choosing the right medical billing company is a critical decision for healthcare providers. With the increasing complexity of insurance policies and regulatory changes, outsourcing your billing processes to a professional medical billing company can help you save time, reduce errors, and maximize revenue. In this comprehensive guide, we’ll discuss how to choose the best medical billing company for your practice and highlight key factors to consider. Also Read: Components of Medical Billing Why Hire a Medical Billing Company? A medical billing company handles the crucial tasks of submitting claims, tracking payments, and following up on denied claims. They also ensure compliance with healthcare regulations such as HIPAA and help streamline the revenue cycle management (RCM) process. Here are some benefits of outsourcing medical billing: Increased Efficiency: Delegating billing tasks allows healthcare providers to focus on patient care rather than administrative duties. Error Reduction: Professional medical billing companies use advanced tools to reduce claim errors and improve reimbursement rates. Cost Savings: Outsourcing eliminates the need to maintain an in-house billing team, reducing overhead costs. Expert Knowledge: Medical billing companies stay updated on regulatory changes, ensuring compliance and accuracy. Also Read: Benefits of Outsourcing Medical Billing Services Key Factors to Consider When Choosing a Medical Billing Company Selecting the right medical billing company requires careful evaluation. Below are the essential factors to keep in mind: Experience and Specialization Look for medical billing companies with extensive experience in your specialty. For example, billing for dermatology differs from billing for cardiology. A company that specializes in your field will understand the nuances of coding and reimbursement, increasing your revenue potential. Technology and Software Ensure the company uses state-of-the-art billing software. Advanced systems like cloud-based platforms improve efficiency, data security, and accessibility. Additionally, confirm that their software integrates seamlessly with your existing electronic health record (EHR) system. Compliance with Regulations Medical billing involves handling sensitive patient information. Ensure the company complies with HIPAA regulations to protect patient data. Ask about their security protocols and data encryption measures. Transparency in Pricing Different medical billing companies have various pricing models, such as: Percentage of Collections: A fee based on the percentage of collected payments. Flat Fee: A fixed monthly rate regardless of collections. Hybrid Models: A combination of both. Request a detailed breakdown of their fees and clarify any hidden charges to avoid surprises. Reputation and References Research the company’s reputation by reading online reviews and testimonials. Ask for references from current or past clients. A reliable medical billing company will have a proven track record of success. Denial Management and Follow-Up Efficient denial management is crucial for maximizing revenue. Ask how the company handles denied claims and whether they have a dedicated team for follow-up. A proactive approach can significantly reduce claim rejection rates. Reporting and Analytics Choose a company that provides detailed reports on your revenue cycle performance. Regular updates and analytics help you monitor trends, identify issues, and make informed decisions. Scalability Your practice may grow over time, so selecting a scalable medical billing company is essential. Ensure they can handle increased billing volumes and adapt to your evolving needs. Customer Support Reliable customer support is vital for addressing concerns promptly. Look for companies offering multiple support channels, such as phone, email, and live chat. Quick response times can make a significant difference. Also Read: Key Features of Medical Billing Services Why Choose RevMax Healthcare? RevMax Healthcare is a leading medical billing company committed to helping healthcare providers optimize their revenue cycle management. Here’s why you should consider RevMax Healthcare: Specialized Expertise: RevMax Healthcare specializes in various medical fields, offering tailored solutions to meet your practice’s unique needs. Cutting-Edge Technology: The company uses advanced billing software to ensure accuracy and efficiency. Transparent Pricing: With competitive pricing models, RevMax Healthcare provides clear and affordable solutions. Compliance and Security: They strictly adhere to HIPAA regulations, ensuring your patient data remains secure. Exceptional Support: RevMax Healthcare offers unparalleled customer support to resolve issues quickly and efficiently. By partnering with RevMax Healthcare, you can focus on delivering quality care while they handle the complexities of medical billing. Also Read: Latest Trends in Medical Billing and Medical Coding Common Mistakes to Avoid When Choosing a Medical Billing Company While selecting a medical billing company, avoid these common pitfalls: Overlooking Compliance: Failing to verify HIPAA compliance can lead to data breaches and legal issues. Ignoring References: Not checking reviews or speaking with other clients can result in poor service. Choosing Based on Cost Alone: While affordability is important, prioritizing cost over quality can harm your practice in the long run. Lack of Communication: Ensure the company’s communication style aligns with your expectations. Neglecting Scalability: Choosing a company that cannot grow with your practice can limit future success. Also Read: Medical Billing vs Medical Coding Conclusion Selecting the right medical billing company is a vital step toward improving your practice’s financial health and efficiency. By considering factors such as experience, technology, compliance, and customer support, you can make an informed decision. Remember to thoroughly evaluate potential companies, ask detailed questions, and request references. If you’re looking for a reliable and experienced medical billing company, RevMax Healthcare is an excellent choice. Their expertise, advanced technology, and commitment to client success make them a trusted partner for healthcare providers. By outsourcing your medical billing to a reputable company like RevMax Healthcare, you can streamline your operations, reduce errors, and maximize revenue—allowing you to focus on what matters most: providing exceptional patient care.